Overview
First Nations people are facing a gap in health outcomes compared to other Queenslanders, particularly in outer regional and remote areas. They need accessible health services that are tailored to their specific needs, including care that is culturally appropriate and based on trust and engagement.
Tabled 7 June 2023.
Acknowledgment
The Queensland Audit Office acknowledges the Traditional and Cultural Custodians of the lands, waters, and seas across Queensland. We pay our respects to Elders past, present, and emerging.
We also thank the many First Nations people and the health workers who generously shared their knowledge and experiences with us during this audit.

Report summary
This audit examines the effectiveness of Queensland Health’s strategies to improve health outcomes for First Nations people. We focused on areas directly within the control of Queensland Health, like how it delivers culturally appropriate health care, its role as a health system manager, and how it manages the challenges of delivering services to First Nations people in remote areas.
Many opportunities to improve health outcomes are beyond Queensland Health’s immediate control, like economic, education, housing, and environmental factors. We do not examine these factors, but we note they present significant challenges requiring sustained focus and coordination across government. Improving health outcomes will also depend on partnerships with other stakeholders, like the community‑controlled health sector.
Queensland Health needs clearer actions to address health inequity
There is a gap between the health outcomes experienced by First Nations Queenslanders and other Queenslanders, particularly in outer regional and remote areas. Queensland Health has committed to addressing these health inequities. To do so, services must be tailored to First Nations people, to meet their specific health needs.
Each hospital and health service (HHS) recently formalised this commitment in health equity strategies. These documents were developed in close partnership with communities and First Nations stakeholders in each region. Most health equity strategies commit to broad and ambitious objectives but do not contain enough detail to explain how the objectives will be achieved.
Each HHS is now publishing health equity strategy implementation plans. It is vital these set out clear and detailed actions to achieve each health equity commitment. Without a clear plan, Queensland Health risks failing to meet its equity commitments and damaging its relationship with First Nations communities.
|
Life expectancy gap 7.8 years for males and 6.7 years for females |
|
|
Potentially preventable hospitalisations 1.6 times greater in First Nations people in remote areas |
|
| 90 per cent of First Nations babies born with a healthy birthweight, compared to 95 per cent for other Queenslanders. |
Queensland Audit Office, from Queensland Health data and estimates.
Queensland Health must improve how it delivers culturally appropriate care
Culturally appropriate care is about delivering services that respond to the needs of First Nations people. It involves building trust and increasing engagement with First Nations people and communities. Queensland Health recognised the importance of culturally capable care in its Aboriginal and Torres Strait Islander Cultural Capability Framework 2010 - 2033 (the framework).
While this 23-year strategy is intended to guide engagement with First Nations people, Queensland Health has not delivered important outputs required under the framework, like regular implementation plans and performance reporting. As a result, it cannot demonstrate how its framework has improved its culturally appropriate care over the last 13 years.
Queensland Health also lacks processes to measure how effectively it delivers culturally appropriate care. For example, it knows more is needed to reduce events that lead to poor health outcomes for First Nations people – like discharging from hospital against medical advice, leaving an emergency department before being seen, and missing specialist outpatient appointments. Stakeholders told us these events can often be explained by a lack of culturally appropriate care.
However, Queensland Health does not assess the root cause of these events for First Nations people and is unable to determine the extent to which culturally appropriate care is a factor. This information is vital to help Queensland Health improve how it cares for First Nations people.

Queensland Audit Office, from Queensland Health: specialist outpatients appointments data; hospital admitted patient data collection data; and emergency data collection.
Having a representative First Nations workforce could improve how Queensland Health delivers culturally appropriate care. Each HHS now has at least one First Nations person on its governing board; most have committed to workforce representation targets; and all offer cultural awareness training to staff.
But there is still a long way to go. Important roles like Indigenous liaison officers are not used consistently, and there are more opportunities to train and develop the non-First Nations workforce to provide better care for First Nations patients.
Better patient travel arrangements are needed
Many First Nations people live in regional and remote areas. Queensland Health’s facilities in these areas are further apart and offer fewer clinical services than in metropolitan areas. This means First Nations patients must often travel long distances to access healthcare.
There is no tailored travel program to help First Nations people in remote areas. While First Nations people can access Queensland Health’s Patient Travel Subsidy Scheme, they may still incur significant out-of-pocket expenses when making long or frequent journeys for health care. Some may avoid or delay travel because of this.
This results in worse health outcomes for the patient and can ultimately cost Queensland’s health system more in the long run. Each HHS can provide additional support to First Nations patients where needed, but this is discretionary and is not publicised.
Each HHS can also do more to help communities understand what services are available to them. A local service catalogue in remote communities would ease confusion about what services are offered by the HHS and other providers in their region.
We make 6 recommendations to improve how Queensland Health works with First Nations people to deliver services. This includes recommendations to improve how each HHS implements its health equity strategies. We also recommend the Department of Health works closely with the HHSs to improve how they deliver culturally appropriate care and help First Nations people access health services.

1. Audit conclusions
Queensland Health (the Department of Health and the 16 hospital and health services – HHSs) can do more to improve health outcomes for First Nations people. First Nations people are still overrepresented in measures that indicate a lack of culturally appropriate care, and providing health care to people in remote communities is an ongoing challenge.
Queensland Health has embedded First Nations leadership, but more is needed to improve culturally appropriate care across the state
Each HHS has displayed a commitment to culturally appropriate care through its First Nations leadership. All HHSs have at least one First Nations person on their governing boards and a First Nations person leading health equity initiatives.
First Nations people are underrepresented in Queensland Health’s workforce across every region. Growing this workforce remains a challenge. It is difficult to recruit and retain suitable staff, particularly in regional and remote areas. There are also challenges in attracting First Nations trainees and graduates with the right skills and qualifications. Queensland Health is currently developing a First Nations health workforce action plan to address this.
Queensland Health is focused on improving how it delivers culturally appropriate care through its health equity agenda. Each HHS has developed new strategies for health equity in its region, but it is too early to tell if these strategies will be effective. Success will depend on how each HHS implements and delivers its commitments. At present, it is not clear how this will be achieved.
Queensland Health has not implemented its cultural capability framework as required
Queensland Health committed to delivering implementation plans every 2 years under its Aboriginal and Torres Strait Islander Cultural Capability Framework 2010 - 2033. The plans were to include strategies, time frames, budgets, and performance indicators for implementing the framework over its 23-year time frame. Queensland Health has not delivered any implementation plans since releasing the framework in 2010.
Queensland Health also committed to fully measuring the success of its cultural capability framework, but it has not developed a system to do this. While it has delivered initiatives under the framework, it cannot demonstrate if these have been effective or how they form part of a coordinated strategy. An independent review in 2018 also recommended Queensland Health address these shortfalls, but the review was not formally actioned.
The Department of Health can do more as a system manager to improve health outcomes for First Nations people
While health services are delivered on the ground across the 16 HHS regions, major changes must also be driven from the centre. The Department of Health (the department) can do more to tackle common issues and evaluate how effectively the health system meets the needs of First Nations people.
The department can do more to measure how effectively Queensland Health delivers culturally appropriate care. While it tracks indicators like missed appointments and discharges from hospital against medical advice, it lacks the information to understand the root causes of these events. As a result, it cannot target its efforts to the areas with the greatest need for improvement.
The department could also act on other system-level challenges. For example, funding for some First Nations health activities is only committed for a year at a time. This limits the ability of each HHS to plan and embed long-term First Nations health initiatives. It can also prevent them from permanently appointing staff to some First Nations health roles, which makes attracting and retaining staff more challenging.
Queensland Health needs to improve access to health services from remote areas
Queensland Health should make it easier for First Nations people to get to hospital. The Patient Travel Subsidy Scheme (PTSS) does not provide adequate support for First Nations people travelling from remote and rural parts of the state.
Accessing the scheme is complex, and the subsidy rates can leave patients significantly out of pocket. Payments are typically made by reimbursement, which can place further financial pressure on patients who travel long distances for health care. While each HHS can provide additional support to patients in need, this is not done through a transparent or consistent process across the state.
Queensland Health has not acted to improve the PTSS. The Department of Health began a reform project in 2017 that identified 32 outstanding recommendations from PTSS reviews, including from the Queensland Ombudsman. The department has not continued this project, and it last reported on it in 2017. Many of these recommendations, if actioned, would improve the experience of First Nations people using the PTSS.
Queensland Health also needs to minimise the need for patient travel by expanding how it delivers services in remote areas. Its new Local Area Needs Assessments have the potential to start this process, but success will depend on how the Department of Health and each HHS work together to meet the health needs of First Nations people across the state.

2. Recommendations
|
We recommend all hospital and health services: |
|
|
We recommend the Department of Health works in partnership with each hospital and health service to: |
|
Reference to comments
In accordance with s. 64 of the Auditor-General Act 2009, we provided a copy of this report to relevant entities. In reaching our conclusions, we considered their views and represented them to the extent we deemed relevant and warranted. Any formal responses from the entities are at Appendix A.

3. First Nations people’s health in Queensland
This chapter is about the health needs of First Nations Queenslanders. We discuss current health outcomes and Queensland Health’s key strategies.
We use the term ‘First Nations people’ in this report to reflect terminology used by Queensland Health. We respect First Nations people’s choice to describe their cultural identity using other terms, such as Aboriginal and Torres Strait Islander peoples, or particular peoples, or by using traditional place names.
We refer to various stakeholders throughout the report. These include:
- First Nations community representatives and health advocates
- clinical staff, including doctors, surgeons, nurses, and other health workers
- health system administrators, including senior First Nations health officials in both the Department of Health and individual hospital and health services.
We provide more detail on our stakeholders in Appendix B.
Our focus and scope
The objective of this audit is to examine the effectiveness of Queensland Health’s strategies to improve health outcomes for First Nations people. We focus on whether Queensland Heath is delivering culturally appropriate care and improving the accessibility of health services for First Nations people.
Queensland Health is Queensland’s public health system. It includes the Department of Health and all 16 hospital and health services (HHSs).
The Department of Health (the department) is responsible for the overall management of the public health system in Queensland, including monitoring the performance of HHSs.
Hospital and health services are statutory bodies, each governed by a hospital and health board. Queensland’s 16 HHSs provide public health and hospital services across the state.
Our audit is limited to Queensland Health entities only. It does not examine the important role played by the community-controlled health sector in Queensland. It also excludes private sector and Australian Government initiatives.
There is a gap between the health outcomes of First Nations people and other Queenslanders
The National Agreement on Closing the Gap (2020) sets out targets for improving the life outcomes and wellbeing of First Nations people. This includes health-specific measures to:
- close the gap between First Nations life expectancy and that of other Australians within a generation, by 2031
- increase the proportion of First Nations babies with a healthy birthweight to 91 per cent by 2031.
We did not assess the rationale behind these targets or Queensland’s progress against them. The following information sets out Queensland Health’s self-reported progress and demonstrates why strategies to improve health outcomes for First Nations people are so important.
Queensland is not on track to close the gap in life expectancy
Queensland aims to close the gap in life expectancy within a generation by 2031. Queensland Health estimates the gap is currently 7.8 years for males and 6.7 years for females. The 3 leading drivers of the gap in life expectancy between First Nations people and other Queenslanders are:
- cardiovascular disease – an estimated 21 per cent of the gap for males and females
- cancers – an estimated 20 per cent of the gap for males and 18 per cent for females
- diabetes – an estimated 13 per cent of the gap for males and 18 per cent for females.
The Queensland Government’s Closing the Gap Snapshot Report 2022 notes life expectancy for First Nations Queenslanders is improving, but Queensland is not on track to close the gap by 2031. Figure 3B shows some of the factors that influence the gap in life expectancy.
Queensland is close to meeting the healthy birthweight target
Babies born full-term and with a healthy birthweight have the best chance of a healthy start to life. Queensland Health reports that close to 90 per cent of First Nations babies were born with a healthy birthweight in 2019, and Queensland is on track to achieve its target of 91 per cent by 2031. Birthweights are also broadly consistent across remote, regional, and the South East Queensland regions.
Avoidable hospitalisations are higher among First Nations people
Potentially preventable hospitalisations are those that could have been avoided if the patient’s condition was better managed. They are not a Closing the Gap measure, but they can directly influence life expectancy. First Nations people experience greater numbers of potentially preventable hospitalisations when compared to other Queenslanders, particularly outside of South East Queensland, as shown in Figure 3A.
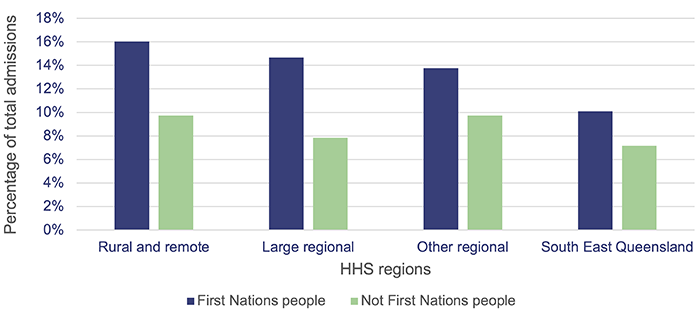
Note: This data reflects patients’ usual places of residence, not where they were treated. HHS regions are set out in Appendix C.
Queensland Audit Office, from Queensland Health’s hospital admitted patient data collection.
Health outcomes are closely connected to other determinants
Health outcomes are directly linked to other social and environmental factors. For example, appropriate housing, availability of healthy food, health literacy, and education all impact on a person’s wellbeing. Figure 3B presents some of the external factors that drive First Nations health outcomes. We did not audit these factors, but we recognise their important role in improving health outcomes for First Nations people.
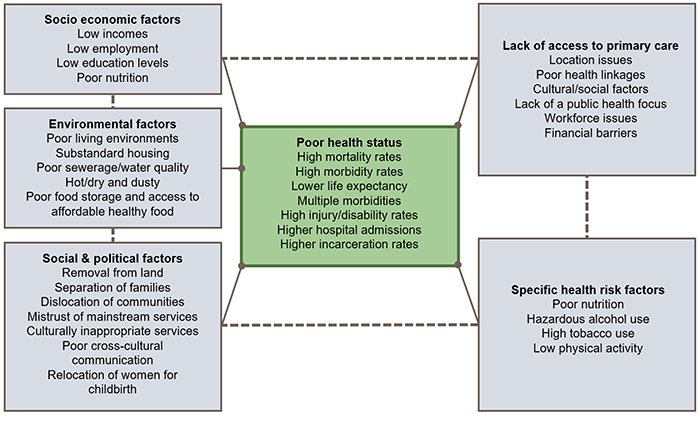
Queensland Health’s Aboriginal and Torres Strait Islander Cultural Capability Framework 2010 - 2033.
Queensland Health’s strategies to close the gap
Queensland Health launched its overarching First Nations health policy, Making Tracks towards closing the gap in health outcomes for Indigenous Queenslanders by 2033: Policy and Accountability Framework, in 2010. Figure 3C details important developments since the implementation of this policy.
Launch of Making Tracks towards closing the gap in health outcomes for Indigenous Queenslanders by 2033: Policy and Accountability Framework
Launch of Aboriginal and Torres Strait Islander Cultural Capability Framework 2010 - 2033
Launch of the Aboriginal and Torres Strait Islander Health Workforce Strategic Framework
Appointment of Queensland’s first Chief Aboriginal and Torres Strait Islander Health Officer and Deputy Director-General
Introduction of requirement to have a minimum of one Aboriginal and Torres Strait Islander person appointed to each HHS’s governing board
Commencement of Hospital and Health Boards (Health Equity Strategies) Amendment Regulation 2021
Launch of Making Tracks Together: Queensland’s Aboriginal and Torres Strait Islander Health Equity Framework
Launch of the HHSs’ inaugural health equity strategies
Queensland Audit Office, from Queensland Health information.
Committing to health equity is a significant step forward
The Queensland Government has committed to addressing health inequities between First Nations people and other Queenslanders. This was formalised by amendments to the Hospital and Health Boards Act 2012 in 2020 and 2021 that set out key health equity requirements for each HHS.
Health equity is about everyone achieving their full health potential
Queensland Health is now adopting a:
… social justice and human rights-based approach to health and healthcare access by redesigning the health system to deliver care based on what First Nations peoples need to attain their full health potential. (Queensland Health’s Making Tracks Together: Queensland’s Aboriginal and Torres Strait Islander Health Equity Framework, 2021)
To achieve health equity, Queensland Health’s services must be tailored to First Nations people and communities to meet individual health needs. This is distinct from equality, which is about providing equal resources to everybody, regardless of their individual needs.
Figure 3D depicts the difference between equity and equality. Using bicycles as an example, it demonstrates how providing the same item to everybody (equality), is not as helpful as giving people different items to meet their unique needs (equity).
Making Tracks Together: Queensland’s Aboriginal and Torres Strait Islander Health Equity Framework, Queensland Health.
Each hospital and health service must explain how it will deliver health equity
All HHSs have published health equity strategies in partnership with First Nations stakeholders in their regions. Each HHS must review and release a new strategy every 3 years and is required to pay for its health equity activities by reprioritising existing funding.
Health equity strategies cover each of Queensland Health’s 5 priority areas:
- actively eliminating racial discrimination and institutional racism in each HHS
- increasing access to healthcare services
- influencing the social, cultural, and economic determinants of health
- delivering sustainable, culturally safe, and responsive healthcare services
- working with First Nations peoples, communities, and organisations to design, deliver, monitor, and review health services.
It is not clear how hospital and health services will implement their health equity initiatives
Most health equity strategies do not contain enough detail to make it clear how they will deliver on their commitments. At face value, many commitments appear hard to achieve without significant investment and focused effort across the health system.
Health equity strategies were developed in partnership with communities, to reflect their views and priorities. While HHSs have made equity commitments that respond to community views, most have not yet developed detailed actions to demonstrate how they will deliver against their commitments.
For example, Figure 3E provides a selection of health equity commitments from various health equity strategies. These commitments address the priority health equity areas, but they are unlikely to be achieved without clear and measurable actions.
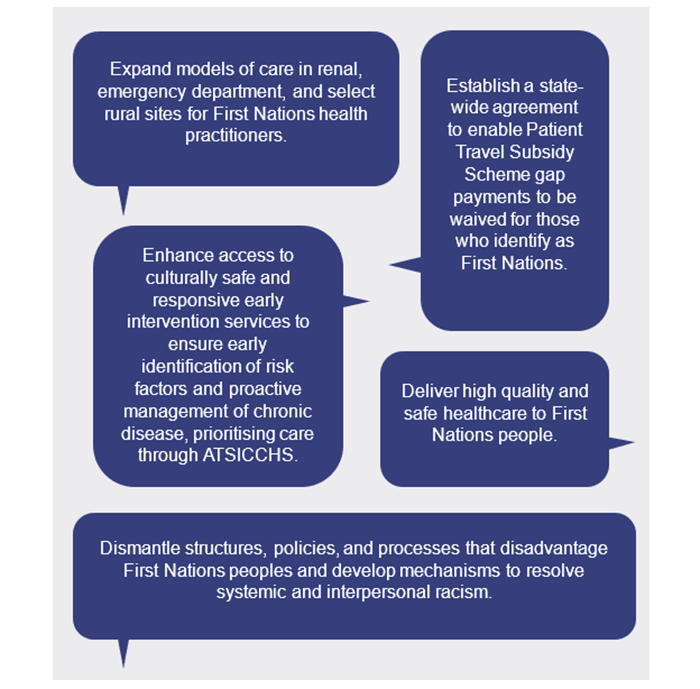
Note: ATSICCHS – Aboriginal and Torres Strait Islander Community Controlled Health Service.
Queensland Audit Office, from hospital and health services’ health equity strategies.
Stakeholders told us |
|
| HHS staff expressed scepticism when asked about their HHS’s ability to deliver on all health equity actions within stated time frames. Other stakeholders were doubtful health equity strategies could make an impact. They noted other government initiatives had been launched with similar enthusiasm but failed to make real change. | |
There is a risk that some HHSs have overcommitted in their health equity strategies. For example, some HHSs have made commitments without securing the necessary funding and staff to deliver them successfully. Others have made commitments that will require significant cooperation with other areas of Queensland Health or the wider health sector. Achieving these will be difficult and may not be within the control of an individual HHS.
If HHSs fail to deliver on their health equity commitments, they risk damaging relationships with their First Nations communities. This ultimately impacts on health outcomes and on Queensland Health’s efforts to close the gap.
Queensland Health needs clear and measurable actions to achieve health equity
Each HHS is now developing a health equity strategy implementation plan in partnership with First Nations stakeholders. These must be delivered in 2023. This is an opportunity to set out clear and costed actions necessary to achieve the health equity commitments. It is vital that these implementation plans include the required level of detail.
Queensland Health’s Health Equity Toolkit recommends implementation plans include:
- implementation timelines
- identification of responsible officers/resourcing
- funding allocations and sources
- strategies to embed into HHS operational plans, and alignment with the operational plans of delivery stakeholders where relevant
- ongoing monitoring and evaluation processes.
Several HHSs have recently published implementation plans, but they do not all contain details on how they will be resourced or what each action will cost.
|
Recommendation 1 We recommend all hospital and health services publish health equity strategy implementation plans that:
|

4. Delivering culturally appropriate care
This chapter is about whether Queensland Health delivers health services to First Nations Queenslanders in a culturally appropriate way. We identify First Nations leadership and workforce representation as factors within the control of each hospital and health service (HHS) that can make a big difference. Our assessment is focused on these areas, but we recognise that improving culturally appropriate care is an ongoing task that extends well beyond the initiatives examined in this chapter.
In this report, we use Queensland Health’s Aboriginal and Torres Strait Islander Cultural Capability Framework 2010 - 2033 (the framework) and other strategies to define terms and inform our findings.
In the context of this report, culturally appropriate care refers to the skills, knowledge, and behaviours that are required to plan, support, improve, and deliver health services in a culturally respectful and appropriate manner. This is sometimes also referred to as ‘cultural capability’.
In this report, all discussion about culturally appropriate care is in reference to the health needs of First Nations people. We do not discuss how Queensland Health delivers culturally appropriate care to other sections of the community.
Queensland Health is committed to improving how it delivers culturally appropriate care, but it does not have a formalised way to measure its progress. Figure 4A summarises 3 indirect measures that could indicate gaps in this.

Queensland Audit Office, from Queensland Health: specialist outpatients appointments data; hospital admitted patient data collection data; and emergency data collection.
Understanding and measuring culturally appropriate care
Culturally appropriate care is not just the absence of racism and discrimination. It is about building a health system that is responsive to the cultural needs of First Nations people. Many factors can limit Queensland Health’s ability to deliver culturally appropriate care.
In some instances, general insensitivity; fear of offending; lack of knowledge of Aboriginal and Torres Strait Islander cultural issues relating to history, spirituality, trauma, loss and grief; and inadequate grounding in health issues and risk factors, prevent Queensland Health from providing quality, culturally appropriate services. (Queensland Health’s Aboriginal and Torres Strait Islander Cultural Capability Framework 2010 - 2033)
Stakeholders told us |
|
|
Some aspects of culturally appropriate care involve significant initiatives, like having influential First Nations leadership across each HHS, or having tailored programs to meet the unique needs of First Nations groups across the state. Stakeholders gave us other examples of effective culturally appropriate care initiatives, such as:
|
|
Culturally appropriate care cannot be directly observed in the same way as clinical outcomes. Many aspects are invisible, like a patient’s sense of safety, comfort, and trust. The consequences of poor culturally appropriate care are also hard to see. For example, a patient who has a poor experience at their HHS may avoid future treatment and could also discourage other community members from engaging with the HHS.
Stakeholders told us |
|
|
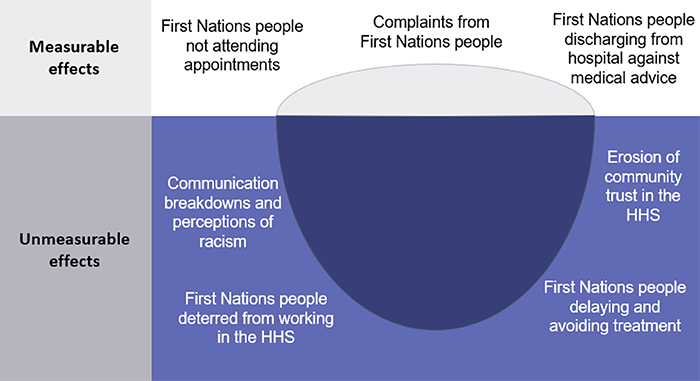
Stakeholders provided examples of some direct and indirect indicators of a lack of culturally appropriate care, depicted in Figure 4B. FIGURE 4B
|
|
Queensland Health has committed to improving how it delivers culturally appropriate care, but has not fully implemented its own framework
Queensland Health’s cultural capability framework recognises the need to improve relationships between Queensland Health and First Nations Queenslanders. The framework provides 4 principles to guide all aspects of its operations:
- cultural recognition and respect
- communication
- relationships and partnerships
- capacity building.
The cultural capability framework includes high-level strategies to embed culturally appropriate care under each of these principles. Queensland Health spent about $42 million between 2010 and 2022 on funding staff and initiatives to improve culturally appropriate care across the health system.
Queensland Health committed to delivering implementation plans under the cultural capability framework every 2 years. The plans were to include strategies, time frames, accountabilities, performance indicators, and budget allocations for implementing the cultural capability framework. It has not delivered any implementation plans since releasing the framework in 2010.
Queensland Health does not fully understand how effectively it delivers culturally appropriate care
Queensland Health has invested significant resources into delivering culturally appropriate care. It needs to be able to measure if its strategies are working so it can make improvements and share lessons across the health sector.
It committed to fully measuring the success of its cultural capability framework but has not implemented a system to do this. It engaged an external provider to evaluate the cultural capability framework in 2018. The provider recommended Queensland Health develop a consistent performance and monitoring framework. It noted that the current performance indicators for cultural capability were useful triggers for further investigation but were not enough on their own.
Queensland Health has not formally actioned the recommendations from the 2018 external review. It advised us it is currently planning a new review on this topic.
A lack of culturally appropriate care can lead to poor health outcomes
In the absence of a formalised measurement process, we discuss 3 possible indicators of gaps in culturally appropriate care – missed appointments, discharges against medical advice, and patient complaints. We selected these because Queensland Health captures data on them. However, we recognise these numbers alone do not explain how, and to what extent, culturally appropriate care is a contributing factor.
Missed appointments may indicate a lack of culturally appropriate care
Queensland Health’s outpatient clinics provide specialist medical and surgical services that do not require hospital admission. They can include diagnostic assessment, screening, treatment, ongoing management, and pre- and post-hospital care.
Patients referred for outpatient services are placed on a waiting list and allocated appointments based on clinical need and availability. HHSs contact patients to offer appointments when they become available.
Depending on need, patients can wait many months for an appointment. For example, our Health 2022 (Report 10: 2022–23) report found the total number of long waits for specialist outpatient services increased by 80 per cent to around 104,000 patients in 2021–22.
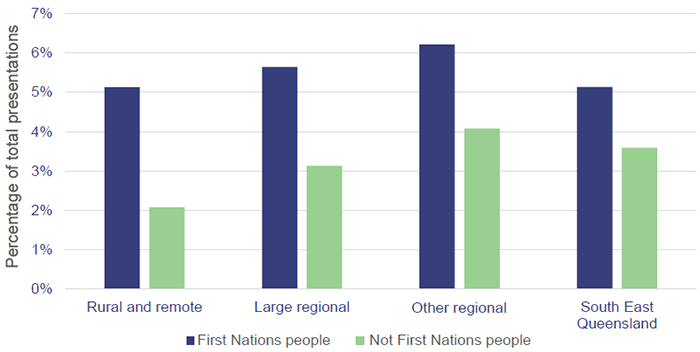
On average, First Nations patients fail to attend appointments at more than double the rate of other Queenslanders. This varies by region and is particularly high for appointments in rural and remote areas, as shown in Figure 4C.
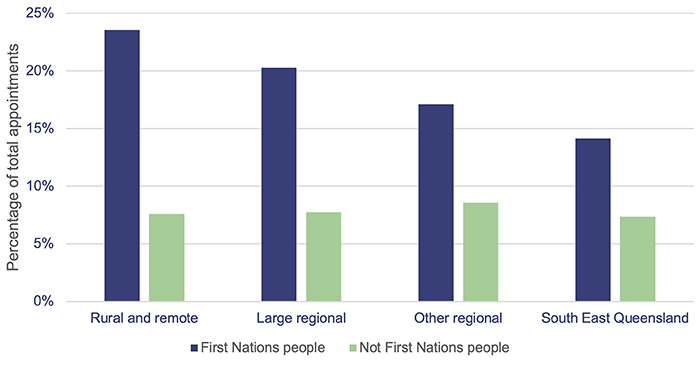
Queensland Audit Office, from Queensland Health specialist outpatients appointments data.
Stakeholders told us |
|
|
Stakeholders explained First Nations people may fail to attend appointments for many reasons, including the challenges of travelling from remote areas. The absence of culturally appropriate care can be another contributing factor. First Nations patients who have had poor experiences with Queensland Health, or who have not been fully informed about the need for further treatment, may be more likely to miss a scheduled appointment. Stakeholders noted these challenges also exist when travelling specialists visit remote communities. Often, patients may not be aware the specialist is in town, or they may need assistance in getting to the local clinic. |
|
Queensland Health does not have the full picture
Reducing the rates at which people fail to attend appointments is a system-wide challenge. While each HHS measures these rates in its clinics, the Department of Health does not routinely collect and analyse this information across the state. For example, it does not know how many First Nations people from remote areas miss appointments in Brisbane. This information is needed to develop strategies that address the issue.
Similarly, Queensland Health does not report on patients who cannot be contacted to schedule an appointment (for example, patients who change their contact details while on the waiting list). HHSs have varied methods to attempt contact with these patients, but it is unclear how many patients go without treatment because they cannot be reached.
Stakeholders told us |
|
|
Stakeholders raised concerns about how Queensland Health communicates with some First Nations patients to offer them an appointment. For example, they noted that sending letters and text messages could be unsuitable for First Nations patients (particularly those in remote communities), who may frequently change address or have unreliable phone service. This would also be of little use to First Nations patients with low English literacy, who may not be able to interpret appointment letters or messages. |
|
More can be done to reduce the number of missed appointments
Each HHS has a process to follow up with patients who do not attend appointments at its outpatient clinics. Queensland Health’s Specialist Outpatient Services Implementation Standard also requires each HHS to have strategies to reduce missed appointments.
Some HHSs take additional steps to contact First Nations patients who fail to attend appointments, like reaching out to the referring clinician or using Indigenous liaison officers where appropriate. Despite this, First Nations people fail to attend appointments in remote and rural areas at close to triple the rate of non‑First Nations patients. This suggests further targeted strategies are needed.
More needs to be done to prevent missed appointments in the first place. Solutions need to be culturally appropriate and developed in partnership with communities. They also need to be accessible across the state, so a specialist outpatient clinic in Brisbane can communicate effectively with First Nations patients in remote parts of Queensland about their appointments.
Stakeholders told us |
|
|
Stakeholders suggested having Indigenous liaison officers or health workers based in communities would be an effective way to communicate with First Nations patients about their appointments. This could involve relaying information about when a patient needs to travel, or if a visiting specialist is in town. Another stakeholder noted social media could be used, with appropriate privacy considerations, to send messages to community members. This could include, for example, public posts on a local health clinic’s page about visiting specialists, or private messages to patients who consent to this contact method. |
|
|
Recommendation 3 The Department of Health works in partnership with each hospital and health service to develop and implement a coordinated strategy to reduce the number of First Nations people from remote and rural areas failing to attend specialist outpatient appointments. This should:
|
First Nations people are more likely to leave hospital against advice
First Nations people leave hospital against medical advice at almost 3 times the rate of non-First Nations people, as shown in Figure 4D. This can present serious risks to their health and welfare and is linked to increased rates of readmission, and greater overall costs to the health system.
Queensland Health closely monitors discharges against medical advice, but it does not have a way to understand how the provision of culturally appropriate care affects this.
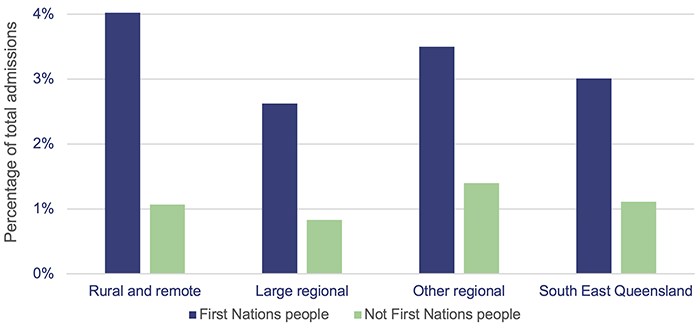
Queensland Audit Office, from Queensland Health’s hospital admitted patient data collection.
First Nations patients are also more likely to leave an emergency department before being treated, as shown in Figure 4E. This is despite being seen within clinically recommended wait times at a greater rate than non-First Nations people.
Queensland Audit Office analysis of Queensland Health’s emergency data collection.
Stakeholders told us |
|
|
Stakeholders told us there are many reasons a First Nations person might leave hospital before completing their treatment. Some reasons include:
Queensland Health could do more to understand and manage these factors, for example, by systematically collecting, and reporting on, the reasons First Nations patients give for leaving. |
|
Queensland Health does not monitor complaints about cultural matters
Patients can complain if they are dissatisfied with Queensland Health's services. Queensland Health advised that it received 1,569 complaints from First Nations people in 2022. The most frequent complaints were about treatment, humaneness and caring, and access and timing.
Queensland Health has a process for managing formal complaints. This involves recording the details of the complaint and investigating and resolving it where appropriate. However, it does not systematically monitor patient complaints data to identify gaps in culturally appropriate care.
For example, it cannot report on all complaints that involve allegations of racism or discrimination. This information could help it to understand trends and systemic issues in how it delivers services for First Nations people.
Stakeholders told us |
|
|
Stakeholders told us many First Nations people do not make complaints despite being dissatisfied with the service they receive at a Queensland Health facility. Some reasons for this include:
Queensland Health could do more to understand First Nations people’s experiences with the health system, for example, by routinely and proactively seeking verbal feedback while patients are in hospital. |
|
|
Recommendation 4 We recommend the Department of Health works in partnership with hospital and health services to implement a systematic way of measuring how effectively Queensland Health delivers culturally appropriate care. This should:
|
A representative workforce can improve culturally appropriate care
Queensland Heath recognises that having a cultural capable workforce is important in improving First Nations health outcomes. It is committed to employing First Nations people, at all levels and in all disciplines, across the state. Each HHS is also required under legislation to have actions in place to grow its First Nations workforce to reflect its local population.
Stakeholders told us |
|
|
Stakeholders stressed the importance of having First Nations workers to provide culturally appropriate care in each HHS. This includes important roles like First Nations health workers, health practitioners, and liaison officers. Increasing the First Nations workforce across each HHS can:
Increasing Queensland Health’s First Nations workforce is likely to improve how the whole health system delivers culturally appropriate care. |
|
Queensland Health is committed to increasing its First Nations workforce
There are many challenges in building and maintaining a representative First Nations health workforce. In the short term, it is difficult to recruit and retain suitable staff, particularly in regional and remote areas. In the long term, there are challenges to attracting First Nations trainees and graduates with the right skills and qualifications.
Queensland Health is developing a First Nations health workforce action plan intended to address the challenges of growing its First Nations workforce. It could not advise when this will be published.
First Nations people are underrepresented in the workforce across every region
Each HHS aims to achieve a First Nations workforce that broadly reflects the size of the First Nations population in its region. This would see a larger proportion of First Nations staff in remote and regional HHSs compared to those in the state’s south-east.
Queensland Health does not have a First Nations workforce that broadly reflects the First Nations population in any region. This disparity is greatest in rural and remote areas, where the gap is 24 per cent, as detailed in Figure 4F.
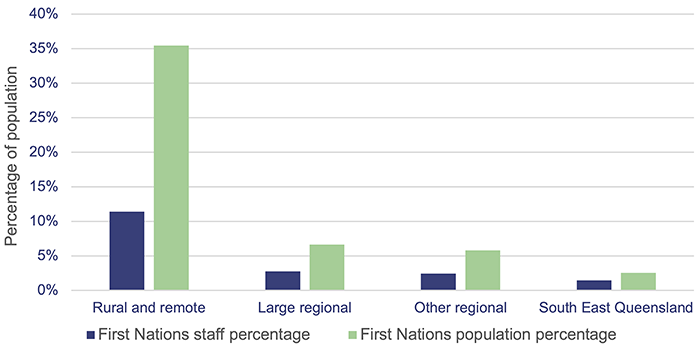
Queensland Audit Office, from Queensland Health’s dashboard and Health needs app data.
Only 10 hospital and health services have a strategy to achieve their First Nations workforce goals
As a starting point to increase the First Nations workforce, HHSs need detailed and practical plans. While 14 of the 16 HHSs have a First Nations workforce target, only 10 have published a strategy to achieve the targets. Figure 4G provides information about each HHS’s First Nations workforce.
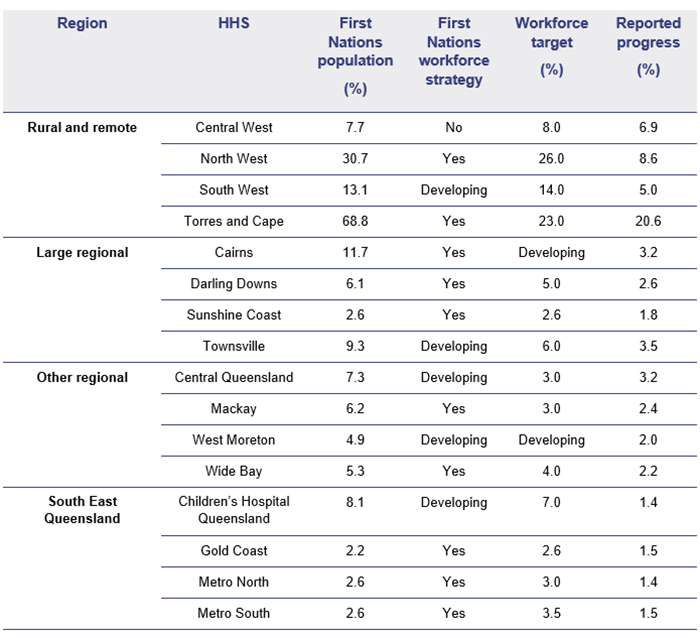
Queensland Audit Office, from Queensland Health data and Queensland Audit Office audit survey response information.
Indigenous liaison officers play a key role
Indigenous liaison officers (liaison officers) are based in most HHSs to provide patient advocacy, education, and support to First Nations patients and their families.
Liaison officers perform broad duties in response to the diverse needs of their First Nations patients. Common responsibilities include:
- routinely visiting First Nations people staying in hospital to provide additional cultural support
- assisting clinical staff to communicate effectively with First Nations people
- assisting families visiting hospital, including for end-of-life events.
Liaison officers told us about the many additional tasks they perform to assist their patients. For example, they frequently help First Nations people with travel arrangements and logistics, like collecting patients from the airport, or helping them to obtain basic food and supplies while they are away from home.
Stakeholders told us |
|
|
Clinical staff emphasised the value Indigenous liaison officers bring to their hospitals. For example, an emergency department clinician praised liaison officers for teaching her team common terms in the local First Nations language. This helped emergency department staff to better understand their local First Nations patients. Another clinician spoke of the valuable on-the-job training liaison officers provide. They noted non-First Nations staff quickly observe how liaison officers engage with patients and model their behaviour on this when appropriate. |
|
Having more Indigenous liaison officers could improve culturally appropriate care
Queensland Health has not defined an acceptable ratio for liaison officers and patients. In some HHSs, like Cairns and Hinterland, liaison officers in 2021–22 had an average of 8 patients to care for each day. Other HHSs, like Mackay, Metro North, Sunshine Coast, and South West, had less than 3 patients per liaison officer each day.
Liaison officers told us their days can be quickly consumed by a single patient, particularly if there is an end-of-life event, or if a patient is wishing to discharge from hospital against the advice of their doctor. In these situations, other First Nations patients may not be able to see a liaison officer if they need to.
There are also no minimum staffing levels for liaison officers across the state, including requirements for liaison officers after hours and on weekends. Liaison officers told us this is not ideal, as patients often need extra support outside of normal business hours.
|
Recommendation 5 We recommend the Department of Health works in partnership with hospital and health services to implement an updated workforce strategy that addresses the key barriers to increasing the First Nations workforce. This should include provisions for recruiting and retaining Indigenous liaison officers, including having:
|
Each hospital and health service must embed systems to deliver culturally appropriate care
Delivering culturally appropriate care is the responsibility of every staff member in each HHS, not just of the First Nations workforce. This is driven from the top by strong First Nations leadership, and from the ground up, through effective training.
All hospital and health services have First Nations board members
Each HHS is independently controlled by a governing board. Boards should contain people with expertise in clinical services, health management, business management, financial management, and human resource management. From 2020, all HHS boards have also been required to have at least one First Nations person.
Each HHS has at least one First Nations person on its board. Five HHSs – North West, Metro North, Torres and Cape, Central Queensland, and Cairns and Hinterland – have appointed 2 or more First Nations board members. This demonstrates their commitment to improving culturally appropriate care.
Executive leadership arrangements vary across the state
Each HHS has a senior officer responsible for First Nations health in its service. Most of these are director or executive director-level positions with oversight of First Nations health initiatives, like the development of health equity strategies.
In some HHSs, Indigenous liaison officers also report to the senior officer responsible for First Nations health. In others, liaison officers report to senior medical staff. This limits routine interactions between the First Nations leaders making administrative decisions and the frontline staff delivering care. Some liaison officers told us they would feel better supported if they reported to a senior First Nations person.
Every hospital and health service offers cultural awareness training
Each HHS uses Queensland Health’s cultural awareness training package. This includes a mandatory online module all new Queensland Health staff must complete as part of their induction training. Some HHSs supplement the online module with additional face-to-face training. This is inconsistent across the state and often depends on when facilitators and staff are available.
Stakeholders told us |
|
|
While the standard online module is a good baseline for all staff, stakeholders told us more frequent and targeted training is needed. For example, administrative and clinical staff who have regular interactions with First Nations patients need training specific to their role. |
|
Training needs to be tailored to various roles across each HHS. This is best delivered on the job, but it needs to be through a structured process that gives each HHS confidence its staff can deliver culturally appropriate care. For example, an adequately resourced Indigenous liaison officer program could provide training across each HHS.
Secure funding is needed to improve how each HHS delivers culturally appropriate care
Queensland Health has spent $790 million on First Nations-specific health programs since 2010 under its overarching First Nations health policy, Making Tracks toward closing the gap in health outcomes for Indigenous Queenslanders by 2033: Policy and Accountability Framework. HHSs received $439 million, non-government organisations received $327 million, universities received $6 million in research grants or payments, and the remainder went to the Department of Health. This funding is used for hospital liaison services, cultural capability programs, development of the health equity strategies, and localised programs.
Making Tracks funding is committed on an annual basis. This prevents HHSs from embedding initiatives to grow the First Nations workforce and improve how they deliver culturally appropriate care. For example, employees in Making Tracks-funded positions cannot be offered permanent, ongoing positions. This makes attracting and retaining suitable staff difficult, particularly in regional areas.
Queensland Health advised that it is moving away from program-based funding for Making Tracks and has made $18.9 million of funding recurrent from July 2023. This is likely to create more stability and certainty, which will help each HHS to commit to and deliver meaningful health equity actions.

5. Accessing health services
This chapter is about the location and availability of Queensland Health’s services across the state. We discuss Queensland Health strategies to help First Nations people access healthcare, particularly in regional and remote areas.
We focus on how First Nations people access health services. We do not examine how Queensland Health is improving access to health services for other sections of the community.
In this report, accessibility refers to the physical location and availability of services offered by Queensland Health across the state.
Many First Nations people travel long distances for health care
Around 4.7 per cent of Queenslanders identify as a First Nations person. The majority live in large regional areas or South East Queensland (65 per cent). While other regional and remote areas have fewer First Nations people in total, they represent a higher proportion of the population in those areas.
Figure 5A provides an overview of where First Nations people live in Queensland.
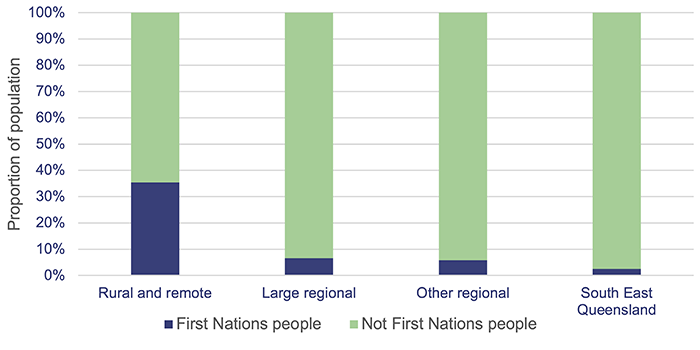
Queensland Audit Office, from Queensland Health data.
There are fewer health services in regional and remote areas
Queensland Health has larger hospitals in 50 locations across the state. The biggest hospitals are in the South East, Townsville, and Cairns. These offer more services and can treat a wider range of conditions than Queensland Health’s smaller facilities.
Queensland Health hospitals in outer regional and remote areas are further apart and offer fewer services. Many parts of Queensland are hundreds of kilometres from a Queensland Health hospital. Some of these areas are serviced by smaller Queensland Health clinics, but patients with complex or serious conditions may need to travel large distances to receive care.
Figure 5B shows the location and clinical capability of Queensland Health’s hospitals. The locations with higher capability levels offer more services across the medical, surgical, emergency, and intensive care categories.
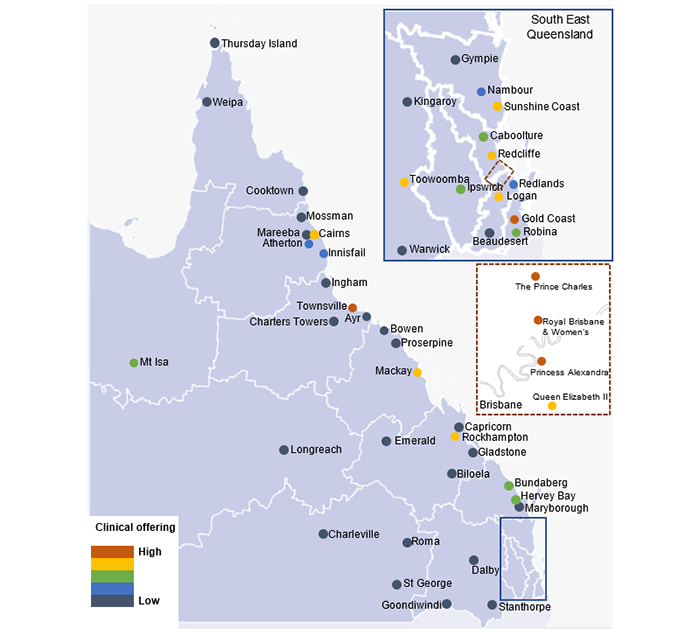
Note: The capability level for each location is an average of Queensland Health’s emergency, medical, surgical, and intensive care unit clinical services capability levels for each hospital and health service. This figure is limited to adult facilities. Children's Health Queensland's facilities are excluded.
Queensland Audit Office, from Queensland Health’s service capability matrix.
First Nations people who most need health care live furthest from it
First Nations people are disproportionally represented in outer regional and remote areas, where they experience poorer health outcomes than non-First Nations people. These are also areas with smaller, less equipped Queensland Health facilities. Around one-third of First Nations patients from remote areas travelled to Queensland Health facilities in larger towns and cities during 2021–22.
Stakeholders told us |
|
|
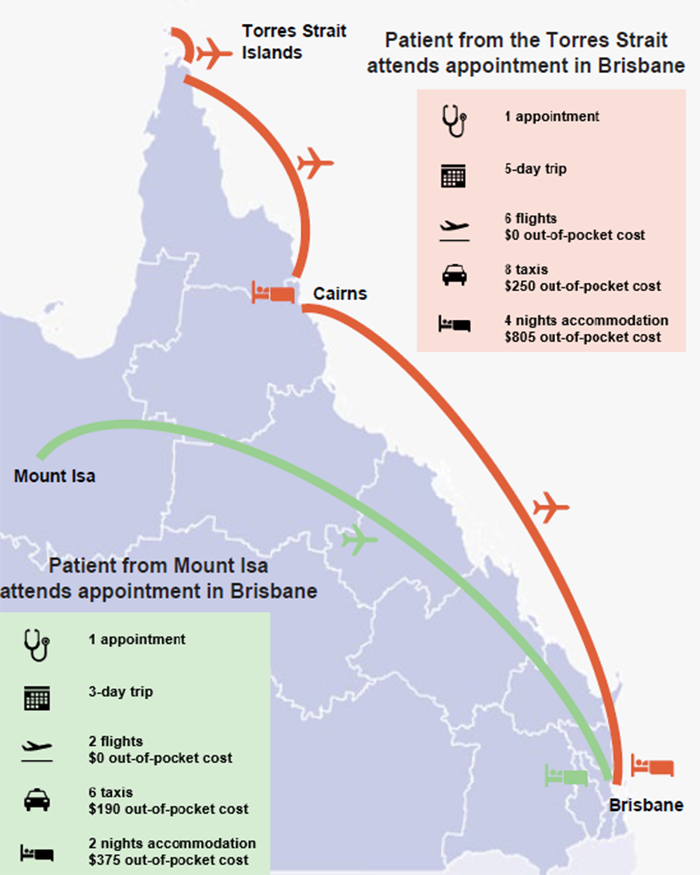
Stakeholders told us about the challenges of travelling for healthcare. Those from remote North Queensland spoke of needing to catch multiple buses to attend hospital. These buses can be infrequent and are often delayed or cancelled due to road conditions. Patients who must travel further for specialist care may need to use air travel. This often requires travelling long distances to a regional centre, like Cairns or Mount Isa, and then flights to Townsville or Brisbane. For example, a patient in the Torres Strait Islands needing treatment in Brisbane could travel around 4,400 kilometres over several days. This is likely to include multiple flights, ferries, and buses. |
|
Queensland Health is working to understand what is needed
Queensland Health is not the only First Nations health care provider in remote and outer regional areas. For example, many regions have a combination of:
- Aboriginal and Torres Strait Islander community controlled health services
- allied health services
- visiting fly-in-fly-out specialists and general practitioners
- mobile primary health clinics.
These services receive a mix of funding from the Queensland Government, the Australian Government, non-government organisations, and the private sector.
Service offerings can change on a regular basis, particularly in remote communities where staffing is difficult to secure. Weather conditions can also impact on services, for example, when towns are temporarily inaccessible or have intermittent essential services.
While Queensland Health has oversight of its own facilities, it does not fully understand what other services are offered in all communities. This makes it difficult to plan services and identify gaps.
Stakeholders told us services can sometimes overlap or be delivered through varying methods. This can frustrate people in communities. They may struggle to understand who is responsible for delivering certain services in their area.
Figure 5C maps the health services in a First Nations community in Queensland. This community has 11 providers delivering 20 different health services, and some services are offered by multiple providers. This is just one example. Different communities may have more or less diversity in service delivery, and things change frequently.
| The service delivery landscape in one First Nations community |
|---|
|
|
Local needs assessments will help map the availability of services
In 2022, each hospital and health service (HHS) was required to publish a summary of its first Local Area Needs Assessments (LANA). The LANA program is designed to assess local health needs across the state, based on data analysis and consultation with local stakeholders, clinicians, consumers, and health organisations.
This differs from Queensland Health’s previous approach to service planning, which focused on demand. While demand is still an important indicator of need, it is not helpful in areas where people do not access health services, perhaps due to the travel required or a lack of health literacy.
LANA assessments provide detail about the local populations of each area, their health status, and the adequacy of existing services. We did not examine the LANA program, but we recognise its potential to improve Queensland Health’s understanding of service delivery needs across the state.
Queensland Health can also use the LANA process to help communities understand what services are available to them and who provides them. A local service catalogue in remote communities would ease confusion about what services are offered by the HHS and other providers in their region.
|
Recommendation 2 We recommend all hospital and health services provide a local service catalogue to communities as part of their Local Area Needs Assessment process. The catalogues should clearly set out what health services are available in each community. |
Patient travel arrangements do not support health equity
The Patient Travel Subsidy Scheme
The Patient Travel Subsidy Scheme (PTSS) provides financial assistance for eligible patients to access specialist medical services that are not available locally. Patients approved for the PTSS receive a subsidy to attend the closest public hospital or health facility where the specialist medical treatment is available. Figure 5D shows the size and scale of the PTSS.
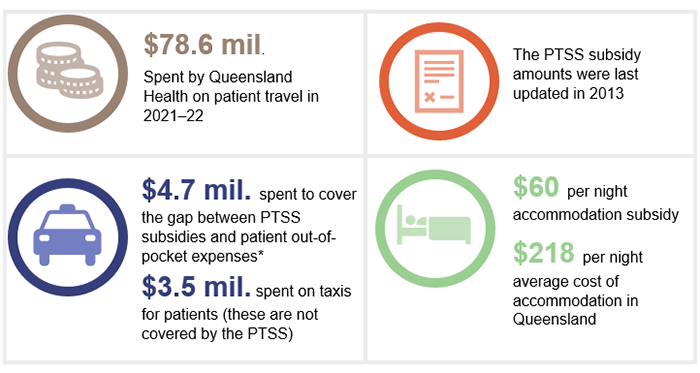
Note: This figure represents all PTSS users, not just First Nations people. *Refers to additional payments made by a HSS to bridge the gap between the PTSS subsidy amount and a patient’s out-of-pocket expenses. This is discretionary and does not include any gap payments made by the patient.
Queensland Audit Office, from Queensland Health financial information; and from the STR Australian Accommodation Monitor Summary for 2021–22. (STR provides global data on the hotel industry.)
Queensland Health does not know how many First Nations people use the Patient Travel Subsidy Scheme
Queensland Health knows its PTSS reporting does not reflect the true number of First Nations people using the scheme. It reports that, in 2021–22, 2.5 per cent of PTSS applications were from people who identified as a First Nations person. This is far lower than the 9.8 per cent admission rate of First Nations people across Queensland in this period.
It is likely that the actual number of First Nations people using the PTSS is far higher than reported. Queensland Health could do more to make its reporting accurate. For example, it could match its figures against admissions data and other sources of information. Having more accurate information would help it to better understand how First Nations people use the scheme.
Stakeholders told us |
|
|
There are many reasons a First Nations person may not self-identify when registering for the PTSS. For example, stakeholders told us a First Nations person may have somebody complete the registration form on their behalf, or they may choose not to identify because they perceive a risk of discrimination. |
|
The Patient Travel Subsidy Scheme process is complex for users
Queensland Health uses a form-based system to administer the PTSS. Many health workers and stakeholders raised frustrations with this process, claiming it is difficult to navigate. This is particularly the case for patients with limited English literacy. Some stakeholders said patients may delay or avoid travelling for healthcare when faced with the PTSS application process.
Figure 5E shows the process each user must complete to access PTSS assistance.
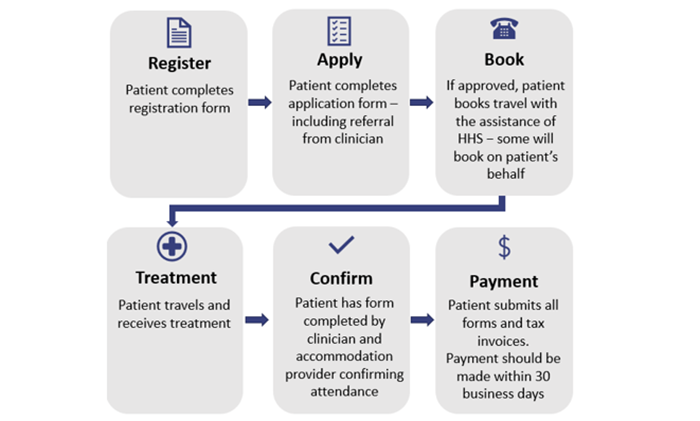
Queensland Audit Office, from Queensland Health information.
The Patient Travel Subsidy Scheme does not cover all costs
PTSS subsidies are not means tested or adjusted for a patient’s income and location. They are also typically paid by reimbursement. This can be challenging for patients who cannot afford the initial expense. The subsidy amounts are outlined in Figure 5F.
|
Expense |
Subsidy |
|---|---|
|
Commercial travel (air, bus, ferry, rail) |
Full cost (cheapest fare) |
|
Private travel (car) |
$0.30 per kilometre |
|
Accommodation |
$60 per night |
|
Travel to/from airport, hospital, and accommodation |
No subsidy |
|
Meals and other incidentals |
No subsidy |
Note: Patients receive no subsidy for the first 4 nights of accommodation in each financial year unless they are a minor or hold a concession card.
Queensland Audit Office, from Queensland Health information.
While the PTSS covers the full cost of commercial travel, the fixed accommodation subsidy of $60 per night can leave patients significantly out of pocket. For example, a patient who needs to stay in Brisbane for care would be out of pocket by $127 per night, based on the average daily rate of accommodation in 2022.
Figure 5G details the average daily rate of accommodation across Queensland and the PTSS subsidy gap.
|
Tourism region |
Average daily rate for accommodation 2022 |
Potential out-of-pocket expense per night |
|---|---|---|
|
Brisbane |
$187 |
$127 |
|
Gold Coast |
$244 |
$184 |
|
Central Qld Coast |
$163 |
$103 |
|
Outback Qld (including Mount Isa) |
$149 |
$89 |
|
Southern Qld Country |
$143 |
$83 |
|
Sunshine Coast |
$279 |
$219 |
|
Townsville |
$153 |
$93 |
|
Tropical North Qld (including Cairns) |
$215 |
$155 |
Note: Potential out-of-pocket expenses have been calculated by subtracting the PTSS accommodation subsidy ($60 per night) from the average daily rate. Actual out-of-pocket expenses may be higher or lower depending on the accommodation rate. Qld – Queensland.
Queensland Audit Office, from STR Australian Accommodation Monitor Summary for 2021–22.
While patients may be able to find accommodation below the average daily rate in each area, it may not have vacancies that match their travel dates. Cheaper accommodation may also be further from health services, requiring non-subsidised taxi or public transport expenses.
Stakeholders told us |
|
|
Patients travelling over multiple days can quickly incur costs. Stakeholders told us many First Nations people cannot afford to travel for healthcare from remote areas, even with PTSS assistance. This can be compounded by family and caring responsibilities, along with lost income if patients take time away from their employment. As an example, Figure 5H shows 2 common trips made by First Nations Queenslanders, detailing their possible out-of-pocket travel expenses. It does not include other expenses like additional food and incidentals. These can accumulate quickly – particularly for people travelling with children. FIGURE 5H
Source: Queensland Audit Office, from Queensland Health information. |
|
There is no process for consistently providing additional support
Queensland Health does not have a formal process for helping patients who cannot afford to travel for health care. However, each HHS can use discretion to further assist patients with travel expenses where needed. In 2021–22, Queensland Health spent $4.7 million to cover the gap between PTSS subsidies and actual accommodation expenses. It also spent $3.5 million on taxis for patients in this period.
Queensland Health’s approach to providing extra travel support lacks structure and transparency. It is not clear how a patient qualifies for further assistance or what support is available. There is also no central guidance for HHS staff to help them provide extra assistance fairly and consistently.
Queensland Health’s current approach relies on a patient disclosing their financial hardship to HHS staff. In practice, many patients are unlikely to request further help unless they are specifically asked to or offered it. Without a transparent process, Queensland Health cannot be confident additional assistance is consistently provided across the state.
Patient travel arrangements do not support health equity
Health equity involves allocating resources to people who need it most. On average, First Nations people in regional and remote areas experience poorer health outcomes and have lower household incomes than other Queenslanders. This group also needs to travel further to receive health care than people in metropolitan and inner regional areas. The current travel system presents real barriers to helping them.
Patients who do not travel to receive necessary health care are likely to experience poor health outcomes. Queensland Health does not know the number of patients who avoid travelling for healthcare due to the cost. For example, it does not monitor or analyse the number of patients who start, but do not complete, a PTSS application. It also does not know how many patients cancel medical appointments requiring travel.
Queensland Health has not acted to improve the Patient Travel Subsidy Scheme
In June 2017, the Queensland Ombudsman investigated Queensland Health’s administration of the PTSS. The Ombudsman noted deficiencies with the administrative operation of the scheme. It also highlighted the need for Queensland Health to address findings and recommendations from previous reviews.
In response to the Ombudsman’s report, Queensland Health began a reform project in 2017 that identified 32 outstanding recommendations from previous reviews of the PTSS, dating back to 2010. These include recommendations to:
- improve patient information and application forms
- develop tools to drive consistent and equitable decision-making
- consider increasing subsidies and allowances.
Queensland Health has not delivered on its reform project and has not reported on the status of the 32 outstanding recommendations since 2017. Many of these recommendations, if actioned, would significantly improve the experience of First Nations people using the PTSS.
|
Recommendation 6 We recommend the Department of Health works in partnership with hospital and health services to improve how it helps First Nations people who must travel for healthcare, including:
|